Rural healthcare systems across the world face persistent challenges that compromise the quality, accessibility, and efficiency of care. These areas often lack specialists, advanced diagnostic tools, and the infrastructure necessary for timely medical interventions. Patients must travel long distances, wait for days or weeks for appointments, and often suffer from delayed diagnoses or treatment. However, with the rapid advancement of healthcare technology, many of these issues are no longer unsolvable. From telemedicine to AI-powered diagnostics, modern digital tools are transforming the way rural populations receive care. Below are ten critical rural healthcare challenges that technology can address effectively.
1. Limited Access to Specialists
One of the most pressing issues in rural healthcare is the lack of medical specialists. For patients needing care from cardiologists, dermatologists, or mental health professionals, the nearest available expert may be located hours away. This often results in delayed consultations and untreated conditions. Technology offers a solution through telemedicine, allowing rural patients to consult specialists via video calls. These platforms enable real-time discussions, sharing of reports, and follow-up care all without requiring the patient to leave their community.
2. Shortage of Healthcare Professionals
Rural hospitals and clinics commonly suffer from a chronic shortage of healthcare workers, including physicians, nurses, and technicians. This limited workforce is often stretched thin, affecting the quality and speed of care delivery. Technological solutions such as AI-powered diagnostic tools, virtual assistants, and clinical decision support systems help automate routine tasks. These tools reduce the burden on staff, ensure consistency in care, and allow healthcare providers to serve more patients efficiently.
3. Geographical and Transportation Barriers
Patients in rural areas often face long journeys over difficult terrain to access basic healthcare. Poor roads, lack of public transport, and seasonal weather disruptions only make things worse. Mobile health units equipped with digital diagnostic tools, combined with telehealth consultations, help bring care directly to the patient’s doorstep. Additionally, virtual consultations reduce the need for travel, enabling timely medical advice and intervention.
4. Inadequate Access to Real-Time Patient Data
In many rural clinics, patient records are still maintained on paper or outdated systems, which hinders the sharing of medical information and delays diagnosis. Cloud-based Electronic Health Records (EHRs) are revolutionizing data management by offering secure, centralized access to patient information. These EHR Software allow healthcare professionals to view a patient’s medical history, lab results, and medications from any location, leading to faster and more accurate clinical decisions.
5. Delayed Emergency Response
Timely medical attention in emergencies like heart attacks or strokes is critical, yet rural areas often lack fast-response systems. Long ambulance wait times and the unavailability of emergency care facilities lead to poor outcomes. Technology can help here through tele-triage systems that connect patients with emergency medical teams in real time. In some cases, drones are even being used to deliver life-saving medications or equipment to remote locations, drastically reducing response times.
6. Limited Diagnostic Capabilities
Rural clinics usually lack advanced diagnostic equipment, resulting in patients being referred to distant cities for essential tests. This leads to delays, increased expenses, and poor follow-up. The emergence of portable diagnostic devices like handheld ultrasound machines, smartphone-based ECGs, and remote pathology tools is making it possible to conduct diagnostic tests even in remote villages. These technologies are not only cost-effective but also help in delivering faster results.
7. Low Health Literacy
Many rural residents struggle to understand medical instructions due to low literacy levels or language barriers. This makes them vulnerable to misinformation and reduces adherence to treatment plans. Technology can bridge this gap through user-friendly mobile health applications that offer educational content in local languages. SMS-based health campaigns and AI chatbots further simplify complex medical information, empowering patients to make informed decisions about their health.
8. Mental Health Stigma and Inaccessibility
Mental health remains a stigmatized and often neglected area of care in rural regions. A lack of mental health professionals combined with social stigma prevents people from seeking help. Telepsychiatry is breaking these barriers by offering confidential consultations online. Mobile apps for mental wellness, therapy, and crisis support also play a crucial role in helping individuals manage their mental health without the fear of judgment or social exposure.
9. Poor Chronic Disease Management
Conditions like diabetes, hypertension, and asthma require ongoing monitoring and management, which is difficult in under-resourced rural setups. Remote Patient Monitoring (RPM) technologies allow patients to measure vital signs at home and transmit the data to healthcare providers. AI algorithms can analyze this data to detect early warning signs, enabling proactive care and reducing hospital admissions.
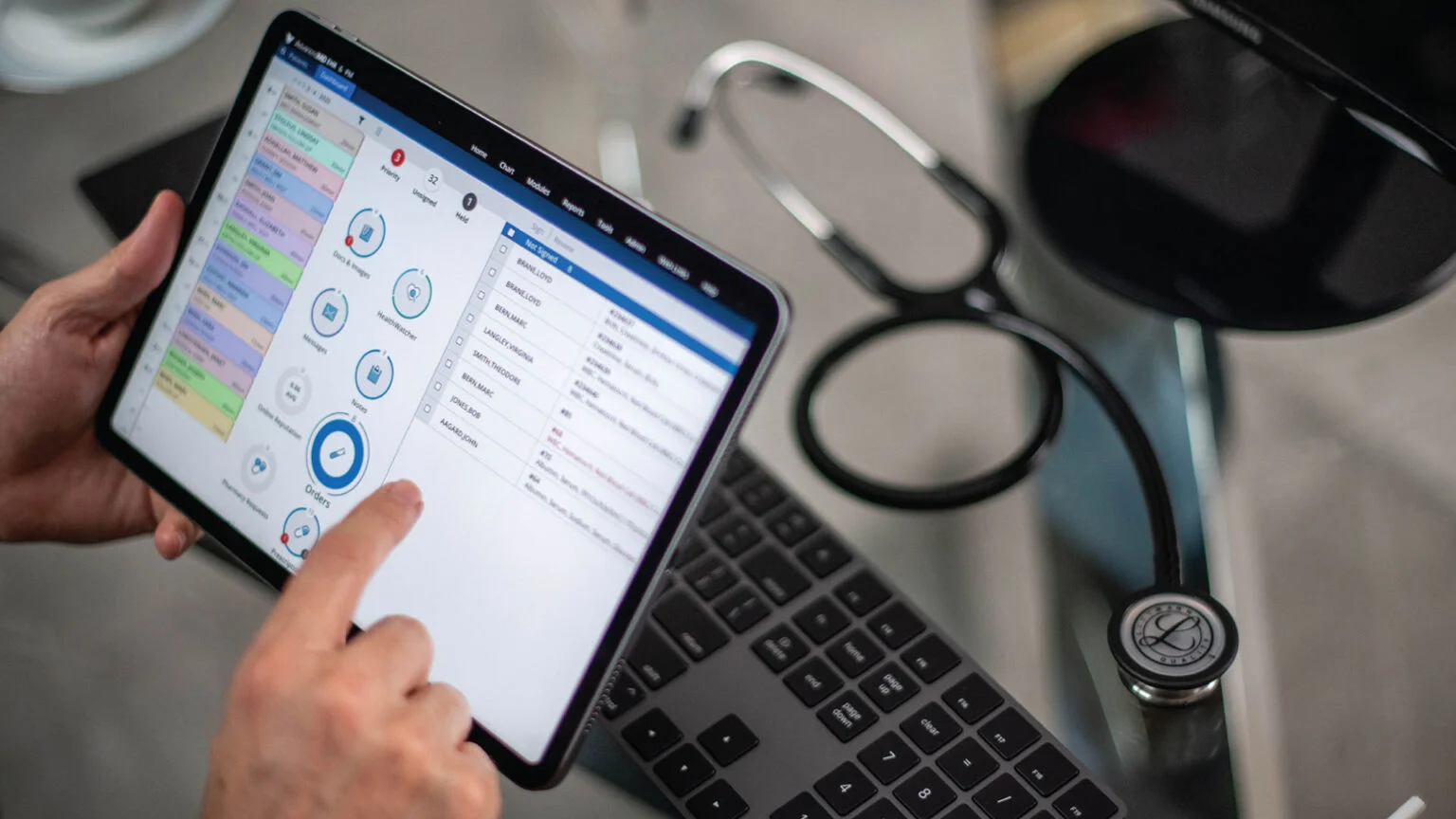
10. Heavy Administrative Burden on Clinics
Small rural clinics often rely on manual administrative processes for billing, inventory, and patient scheduling, which increases human error and consumes valuable time. Implementing Clinic Management Software automates these tasks, leading to more organized operations and improved patient experiences. With features like automated billing, digital prescriptions, and appointment reminders, these systems help clinics focus more on clinical care and less on paperwork.
Conclusion
Technology is not a cure-all, but it is a powerful enabler for overcoming rural healthcare challenges. By leveraging digital tools like Clinic Management Software, rural clinics can enhance access, improve care quality, and operate more efficiently. However, successful implementation also requires investment in infrastructure, internet access, and digital literacy training for both patients and providers. If supported by thoughtful policies and community engagement, technology can play a transformative role in ensuring that quality healthcare is not a privilege limited to urban centers, but a right available to every citizen, regardless of geography.